Science
UBC Breakthrough Transforms Kidney Transplant With Enzyme Technology
The University of British Columbia (UBC) has achieved a significant breakthrough in organ transplantation, successfully converting a kidney from blood type A to the universal type O using specialized enzymes. This landmark development was published in the journal Nature Biomedical Engineering and represents a promising advance in the quest to provide kidney transplants to thousands of patients more rapidly.
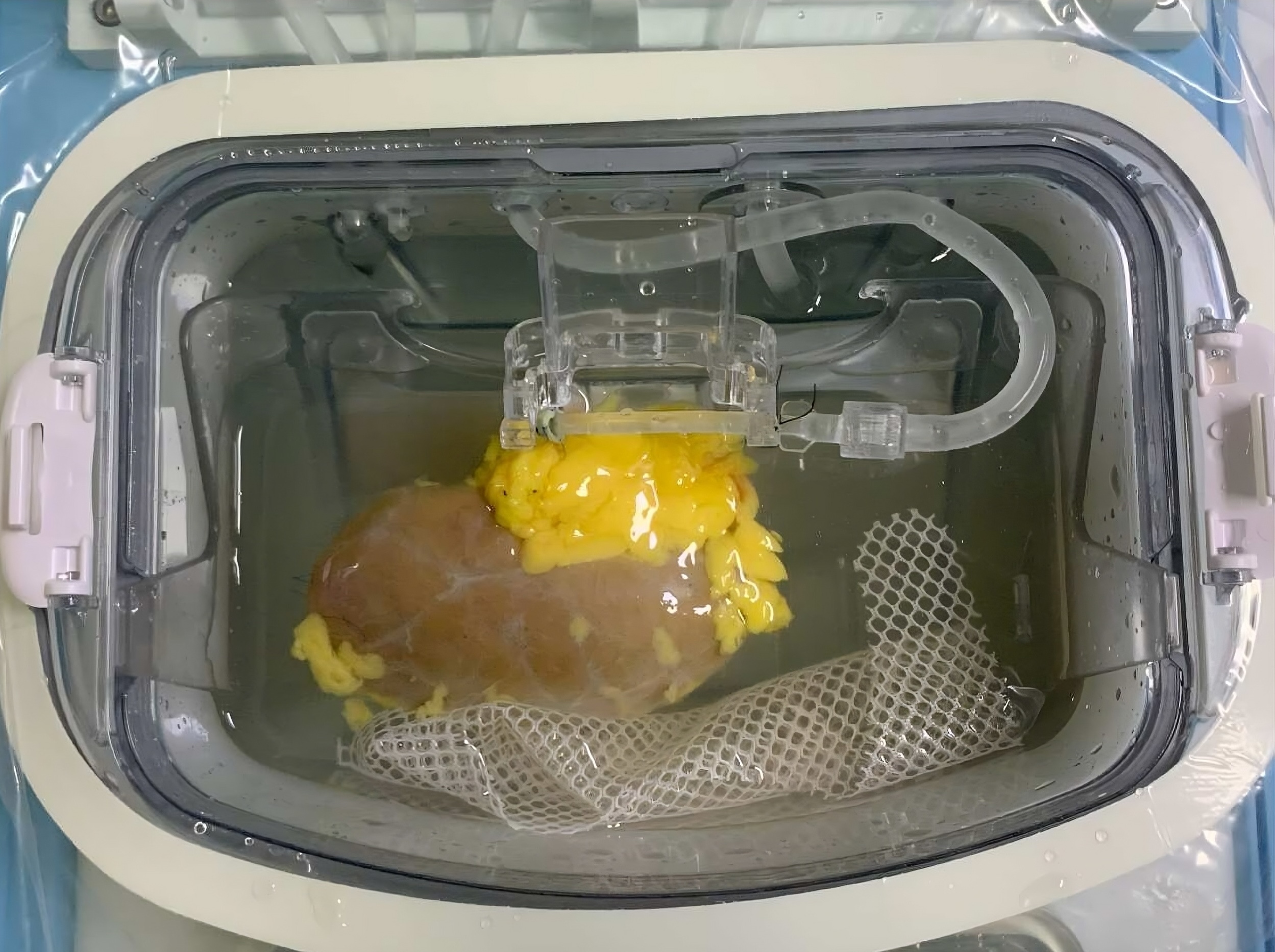
In a pioneering experiment, the enzyme-treated kidney was transplanted into a brain-dead recipient with family consent. This approach allowed researchers to monitor the immune response without jeopardizing a living patient. Remarkably, the kidney functioned for two days without any signs of hyperacute rejection, a rapid and often fatal immune reaction that can destroy an incompatible organ within minutes. By day three, some blood-type markers began to reappear, leading to a mild immune response. However, the damage was significantly less severe than typically observed in mismatched transplants, indicating that the recipient’s body was starting to accept the organ.
“This is the first time we’ve seen this play out in a human model,” stated Dr. Stephen Withers, UBC professor emeritus of chemistry and co-leader of the enzyme development project. “It gives us invaluable insight into how to improve long-term outcomes.”
The development of this technology stems from over a decade of research. In the early 2010s, Dr. Withers, alongside colleague Dr. Jayachandran Kizhakkedathu, focused on creating universal donor blood by removing the sugars that define blood types. These sugars, known as antigens, also coat the blood vessels of organs. If a recipient’s immune system recognizes an incompatible antigen, it triggers an attack on the organ.
Patients with type O blood, who make up more than half of the kidney transplant waitlist, can only receive kidneys from type O donors. Unfortunately, type O kidneys are frequently allocated to other blood types due to their universal compatibility, leading to extended wait times of two to four years for type O patients, many of whom do not survive the wait.
Traditional methods to address blood-type incompatibility involve extensive treatments to strip antibodies and suppress the recipient’s immune response, often requiring organs from living donors. The innovative UBC approach not only alters the organ itself but also promises to expedite transplant procedures, reduce complications, and allow for the use of organs from deceased donors, where every moment can be critical.
The core of this technology lies in a discovery made by the UBC team in 2019, when they identified two highly efficient enzymes capable of removing the defining sugar of type A blood, effectively converting it to type O. “These enzymes are highly active, highly selective, and work at very low concentrations,” explained Dr. Kizhakkedathu. “That made the whole concept feasible.”
The next challenge was applying this technology to entire organs, a hurdle overcome in 2022 when a team in Toronto successfully demonstrated the conversion of lungs. Following successful tests on blood, lungs, and kidneys outside the body, the researchers sought to determine if an enzyme-converted organ could survive in the human immune system.
The answer came in late 2023 during an overseas visit by Dr. Kizhakkedathu, when collaborators demonstrated the successful conversion and transplantation of a human kidney. “I was so thrilled. It was a dream moment,” he recalled, expressing his excitement upon learning the kidney was functioning well.
The UBC enzymes act as molecular scissors, effectively removing the ‘nametag’ that identifies type A blood and revealing type O beneath. “It’s like removing the red paint from a car and uncovering the neutral primer,” Dr. Withers remarked. “Once that’s done, the immune system no longer sees the organ as foreign.”
The next steps include obtaining regulatory approval for clinical trials, with UBC’s spin-off company, Avivo Biomedical, leading the development of these enzymes for transplantation applications. The implications of this research are vast, paving the way for the creation of universal donor blood on demand for transfusion medicine.
“This is what it looks like when years of basic science finally connect to patient care,” Dr. Withers stated. “Seeing our discoveries edge closer to real-world impact is what keeps us pushing forward.”
-

 Science2 months ago
Science2 months agoToyoake City Proposes Daily Two-Hour Smartphone Use Limit
-

 Health2 months ago
Health2 months agoB.C. Review Reveals Urgent Need for Rare-Disease Drug Reforms
-

 Top Stories2 months ago
Top Stories2 months agoPedestrian Fatally Injured in Esquimalt Collision on August 14
-

 Technology2 months ago
Technology2 months agoDark Adventure Game “Bye Sweet Carole” Set for October Release
-

 World2 months ago
World2 months agoJimmy Lai’s Defense Challenges Charges Under National Security Law
-

 Technology2 months ago
Technology2 months agoKonami Revives Iconic Metal Gear Solid Delta Ahead of Release
-

 Technology2 months ago
Technology2 months agoSnapmaker U1 Color 3D Printer Redefines Speed and Sustainability
-

 Technology2 months ago
Technology2 months agoAION Folding Knife: Redefining EDC Design with Premium Materials
-

 Technology2 months ago
Technology2 months agoSolve Today’s Wordle Challenge: Hints and Answer for August 19
-

 Business2 months ago
Business2 months agoGordon Murray Automotive Unveils S1 LM and Le Mans GTR at Monterey
-

 Lifestyle2 months ago
Lifestyle2 months agoVictoria’s Pop-Up Shop Shines Light on B.C.’s Wolf Cull
-

 Technology2 months ago
Technology2 months agoApple Expands Self-Service Repair Program to Canada









